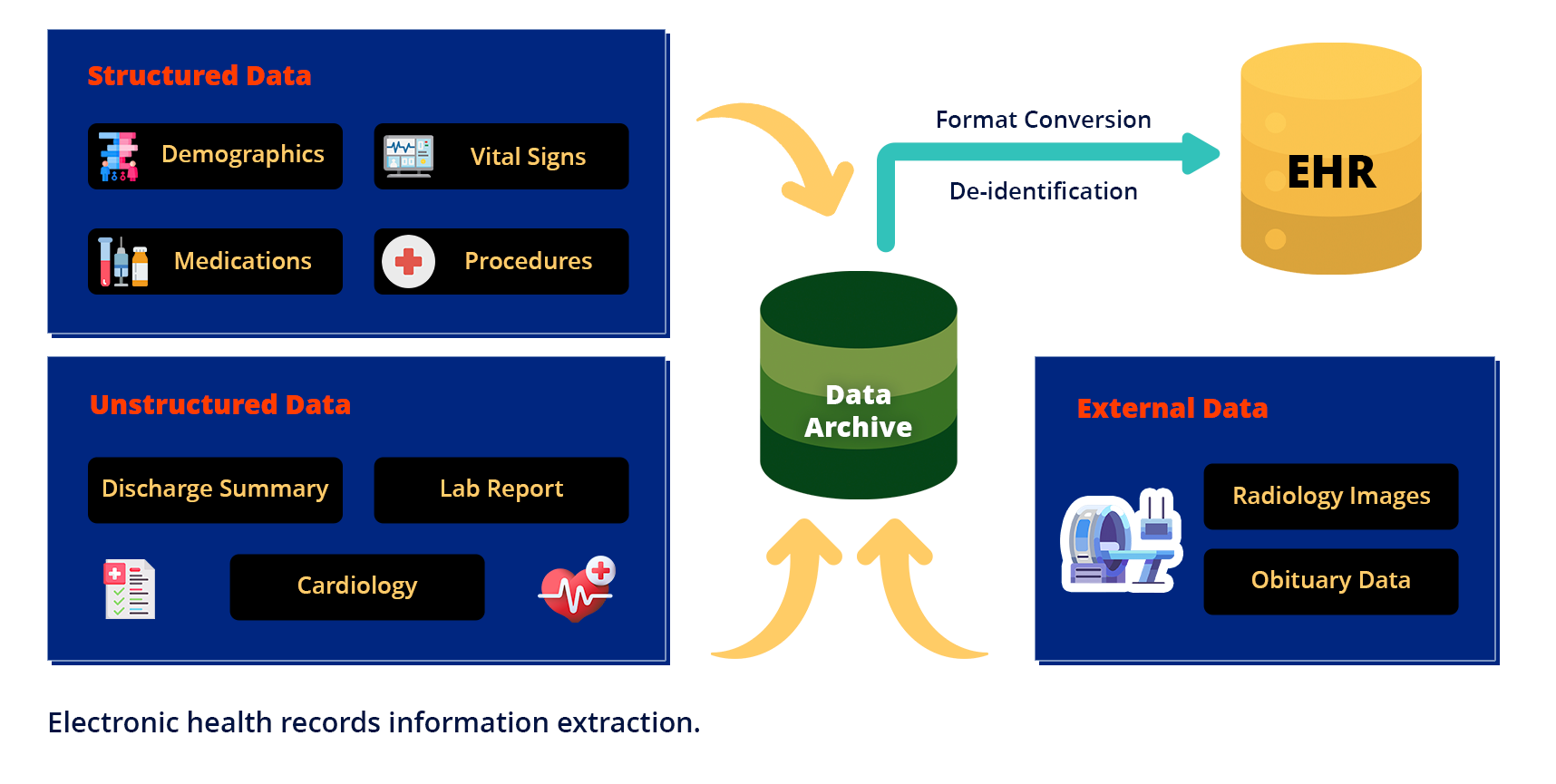
EMR data extraction can be a complex task. Apart from the wide range of options available to you, your EMR contains a mixture of structured and unstructured data.
In the rapidly advancing world of healthcare, Electronic Medical Records (EMRs) and Electronic Health Records (EHRs) have become essential tools for managing patient information. These digital systems store vast amounts of data, from patient histories to treatment plans, offering a treasure trove of insights for improving care and operational efficiency. However, the true potential of this data lies in its extraction—pulling it from legacy or current systems and transforming it into actionable knowledge. This article dives into the importance of EMR/EHR data extraction, the challenges it addresses, and how it can revolutionize healthcare delivery.
While most EMR data extraction activities require pulling data from normalized, structured data elements, there’s a significant volume of unstructured data that must not be ignored. The first step in obtaining existing legacy patient data, proper EMR data extraction, means exporting as much data as possible in a usable format in order to seamlessly migrate to the new system.
- What is EHR data extraction?
- Why is EHR/EMR Data Extraction important?
- Methods of EMR/EHR Data Extraction
- How to Get Started with EMR/EHR Data Extraction
- What is structured and unstructured healthcare data ?
- How is legacy EMR data extracted?
- Challenges in EHR/EMR data extraction
What is EHR Data Extraction?
EHR data extraction is one of three essential alternatives to move all data from a legacy EHR system to a new system and is done through a process known as ETL. During this process, patient data is EXTRACTED from the legacy system, TRANSFORMED to align with the map created for the new system, and LOADED into the new system.
Why EMR/EHR Data Extraction Matters?
Healthcare organizations rely on data to drive patient outcomes and streamline operations. Yet, many are stuck with legacy systems that hinder progress. Extracting data from these platforms unlocks several key benefits:
- Overcoming Legacy System Limitations– Legacy EMR/EHR systems often lack modern features like interoperability, telemedicine integration, or robust analytics. Extracting data allows organizations to move to advanced platforms that support current healthcare needs, ensuring they stay competitive and compliant.
- Enhancing Patient Care- Extracted data provides a comprehensive view of patient histories, enabling clinicians to make informed decisions quickly. For example, pulling lab results or past diagnoses into a new system ensures continuity of care during transitions, reducing the risk of errors.
- Boosting Operational Efficiency–Manual data entry from old records is time-consuming and error prone. Automated extraction streamlines workflows by transferring data seamlessly, freeing staff to focus on patient care rather than administrative tasks.
- Strengthening Data Security– Outdated systems are prone to security vulnerabilities due to unsupported software or weak encryption. Extracting and migrating data to secure, cloud-based EHRs enhances protection against breaches, aligning with regulations like HIPAA.
- Enabling Research and Insights– Extracted EMR/EHR data fuels analytics, helping providers identify trends, improve treatments, and contribute to clinical research. From structured datasets to mined unstructured notes, this information drives evidence-based practice.
Methods of EMR/EHR Data Extraction
Several techniques make data extraction efficient and reliable, depending on the system and goals:
- Application Programming Interfaces (APIs)– APIs allow structured data to be pulled directly from an EHR into another system or archive. They’re fast, standardized, and ideal for interoperable platforms, simplifying transfers between providers or to patient portals.
- Natural Language Processing (NLP)– For unstructured data like clinical notes, NLP algorithms extract meaningful insights—such as diagnoses or symptoms—by analyzing text. This method unlocks valuable information that structured fields alone can’t provide.
- Optical Character Recognition (OCR)– When dealing with scanned documents or PDFs in an EMR, OCR converts images into editable text. While it requires human oversight to correct errors, it’s a vital tool for digitizing older records.
- Custom Scripting– For unique or legacy systems, custom-coded tools can extract data when standard methods fall short. This approach demands technical expertise but offers flexibility for complex migrations.
Turning Extracted Data into Action
Once data is extracted, its potential is limitless. Migrating it to a modern EHR enhances daily operations, while archiving it ensures long-term access for compliance or audits. Active archiving solutions, for instance, keep historical data accessible without overloading new systems, reducing costs and claim denials. Meanwhile, feeding extracted data into analytics tools uncovers trends that improve care delivery and inform strategic decisions.
How to Get Started with EMR/EHR Data Extraction ?
- Define Goals: Decide if you’re migrating, archiving, or analyzing data to guide the process.
- Assess Systems: Evaluate your current EMR/EHR for data types and extraction challenges.
- Choose Tools: Select APIs, NLP, or expert vendors based on your needs.
- Partner with Experts: Work with specialists like Triyam to ensure accuracy and compliance.
- Validate Data: Check extracted data for integrity before full implementation.
What is Structured and Unstructured Healthcare Data?
Healthcare organizations rely on the power of data to improve operational efficiency and gain valuable insight into patient health and treatment. However, of the volume of data that is available, only 10% – 20% of it is usable. As a result, 80% – 90% of healthcare unstructured data is not leveraged because it is too challenging to interpret.
Structured data is often managed and searched through an online database or through an online database management system (RDBMS). This includes integers, decimals, dates, time, strings, and Booleans. These information varieties are unit simply organized in rows and columns and may be queried by victimization programming languages like SQL to come back with relevant search data. They will be mechanically combined and processed as a result of their easy boundaries and are made and kept in a standardized format.
Examples of Structured Data in Healthcare
In care, structured information is preponderantly wont to record patient data in electronic health records (EHR). Here area unit some examples:
- Medical take a look at results are often recorded within the variety of a numeric or Boolean worth.
- Physical measures like height, weight, pressure level, blood type, and stage of the sickness are often recorded numerically.
- Dropdown menus are often used for storing demographic data.
- A radio button can be used to denote the patient’s gender, marital status, and other binary values.
In every example, what makes the values structured is the ease with which they will be parsed by computers and queried by humans. In an endeavor to create clinical information, even a lot of uniform and accessible comes just like the Structured Data Capture (SDC) Profile has provided associate infrastructure for capturing, exchanging, and utilizing EHR information to enhance clinical analysis, enhance adverse event coverage, and optimize public health coverage.
Unstructured data, on the other hand, isn’t computer code and thus needs extended pre-processing in preparation to be used with analysis tools.
Unstructured Data Examples in Healthcare
Unstructured health data remains one of the most precious and untapped resources in the healthcare ecosystem. While determined medical professionals can certainly make use of this data, the process is time-consuming and fails to produce an overall, cohesive picture. Here are some examples of unstructured data:
- Medical images such as PET, CAT, and MRI scans, X-rays, and ultrasounds.
- Audio recordings from therapy sessions.
- Text files of varying lengths, such as medical notes and evaluations.
How is Legacy EMR Data Extracted?
Legacy systems in healthcare such as Electronic Health Records (EHRs) and Electronic Medical Records (EMRs) software companies want to convince you that you must keep paying subscription fees to maintain access to your facility’s legacy data. The truth is the information is yours. Learn how to easily extract legacy data and transfer it into an easily accessible format.
Legacy systems in healthcare are dangerous. Legacy systems in healthcare such as Electronic Health Records (EHRs) and Electronic Medical Records (EMRs) software companies want to convince you that you must keep paying subscription fees to maintain access to your facility’s legacy data. The truth is the information is yours. Contact us to learn how to easily extract legacy data and transfer it into an easily accessible format.
- System integrity – Legacy systems still require annual subscription fees, but archaic platforms are less likely to be continuously upgraded. The original software developers may not be at the company and even if they are, they are working on the latest version rather than the old system. This means that the integrity of the entire system and its data is at risk from cyberattacks and hardware failures.
- Access to information – You know passwords can be lost, new staff aren’t trained on old systems, or previous hardware is housed elsewhere. These situations make auditing and legal requests for information an administrative nightmare. The legislation mandates access to information for up to 10 years, so you need quick access to archived information.
- Patient care – Technically this is also access to information, but the only reason medical facilities exist is to help patients. Patients sitting in examination rooms suffer (or complain!) when information is restricted to those who have passwords and access to the system
Challenges in EHR / EMR Data Extraction
Data access and privacy – Due to the high sensitivity of data collected by EHR systems, access to clinical data such as electronic medical records is highly restricted. Ethical clearance is required, as well as good communication with healthcare providers. The reuse of such data for research and quality improvement work is subject to multiple levels (GDPR (2016), HIPAA (2003), and national and institutional policy). At the same time, there are forces demanding that the valuable information available within the healthcare system be used not only for research but also for improving healthcare.
Data quality is a major issue and we need ways to improve data integrity, compliance, and validity.
Statistical analysis – Data collected from EHRs may have higher error rates than data collected using proprietary systems and subjected to “cleansing” and validation. Missing data, including those resulting from cluster-wide failures, pose certain problems for PCT. Preliminary data collection and evaluation provide an indication of whether a proposed study is viable given data availability and quality.